6 January, 2021
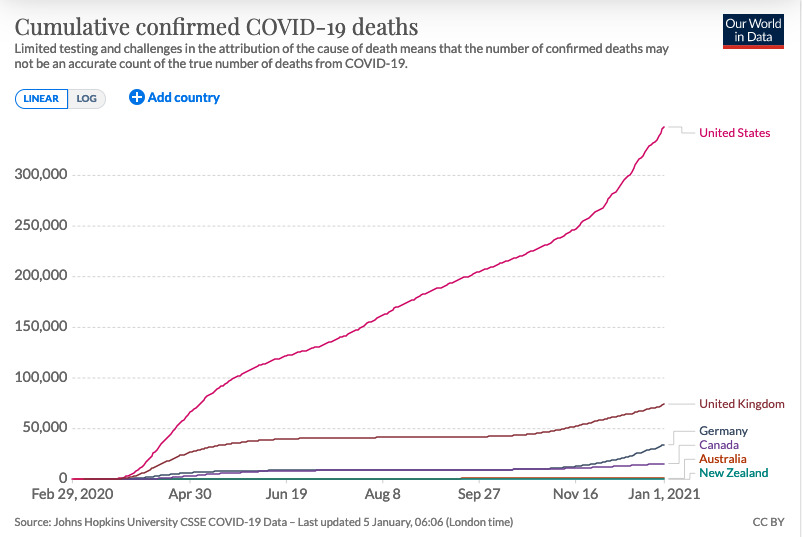
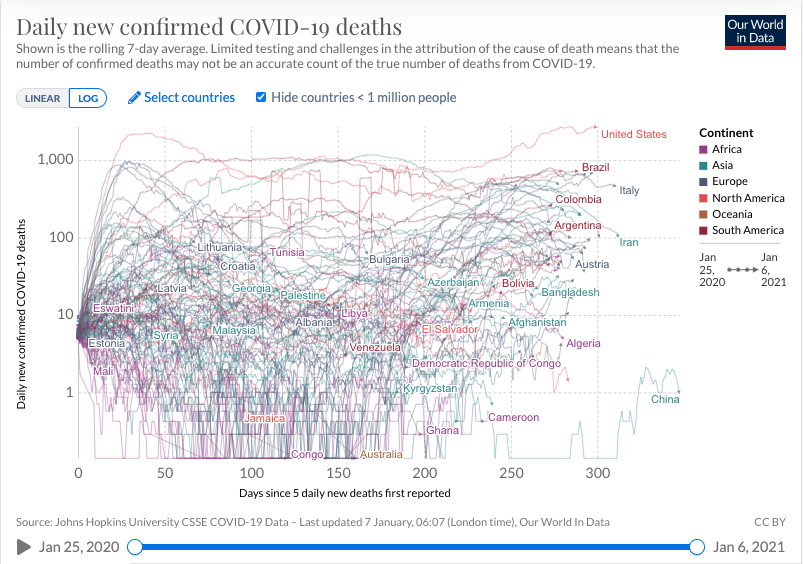
COVID-19 remains a serious safety risk for rowers as the United States continues to have one of the highest numbers of confirmed deaths, the highest number of confirmed cases, and the highest numbers of cases and deaths per capita, among the countries of the world.
At the same time the COVID-19 virus continues to mutate; it has become apparent that it can infect people of all ages, including healthy young adults; and there may be long-term cognitive effects from even mild infections.
27 July 2020
At least twelve members of the US National Rowing Team contracted COVID-19 at the NJ training center in March. As Olympic gold medalist Emily Regan was quoted in an article published by the New York Times “the narrative that has been going around in some places is that you won’t get the virus if you’re young and strong, or if you get it, it won’t be bad, but we’re perfect examples of how that is totally not true… Look what the virus still did to us. It knocked us down pretty hard.” [italics added]
Although the cases were categorized as mild by the team doctor, and the athletes were all world class competitors with outstanding lung capacity and efficiency, some athletes were still dealing with complications more than forty days after the onset of the disease, and still trying to get back in competitive shape more than three months later.
24 July 2020
With the resurgence of confirmed COVID-19 cases and deaths throughout the US in June and July, more attention is being given to warnings of continued contagion into the fall and winter, and the possibility that these may coincide with seasonal flu infections. A forthcoming book by epidemiologist Rob Wallace reminds us that “H1N1, H7N9, SARS, MERS, Ebola Makona, Zika, and a variety of lesser viruses have emerged almost annually,” and there is good reason to believe that such mutations will continue in coming years as a consequence of changes in the global environment.
6 July 2020 Update
The Washington Post is reporting today that more than 200 scientists from around the world have expressed concerns to the World Health Organization about “growing evidence that the (COVID-19) virus can spread indoors through aerosols that linger in the air and can be infectious even in smaller quantities than previously thought.” (italics added)[https://rowsafeusa.org/wp-admin/post.php?post=1603&action=edit]
4 July 2020 Update
There is increasing evidence that the overwhelming number of COVID-19 infectious transmissions occur indoors — not outdoors. Dr. Gabe Mirkin reports that in one study only two of 1245 cases occurred in outdoor environments. HOWEVER, he writes, “a study reported in Emerging Infectious Diseases (July, 2020;26(7)) found that:
• The virus was widely distributed on floors, computer mice, trash cans, sickbed handrails and other surfaces, and was detected in the air 12 feet from patients…
• Floors… were loaded with virus, because gravity settles the respiratory droplets there.
• Fifty percent of the shoe soles of medical personnel were covered with virus.
• Masks were loaded with virus — a sign that they are working, but need to be washed or discarded after every use.”
The lesson for rowers in this is that rowing outdoors doesn’t present significant COVID-19 risks; warming up, working out, and milling around inside the boathouse does.
1 June 2020 Update
A comprehensive, interactive, state-by state compendium of restrictions on social activities relating to COVID-19 is available at the Council of State Governments (https://web.csg.org/covid19/).
[12 May 2020 Update]
Federal and State Restrictions on Social Activities
- COVID-19 restrictions have now been relaxed by the federal government and thirty states. This may allow clubs and teams to resume rowing in many states.
- The White House criteria for relaxing social restrictions are:
- A downward trend of flu-like illnesses within a 14-day period;
- A downward trend of COVID like cases within a 14-day period;
- A downward trend of documented COVID cases OR
- A downward trend of the percentage of COVID cases within a 14-day period;
- The ability of hospitals to treat all patients without crisis care;
- Robust testing for at-risk healthcare workers.
- None of those thirty states currently meet the White House criteria for reopening.
Public Health Concerns about Premature Resumption of Social Activities
- Premature resumption of social activities poses serious risks because:
- the disease remains highly contagious and can be transmitted by asymptomatic people
- Unlike most viruses, SARs-CoV-2 is both highly contagious and potentially lethal
- Widespread testing is not yet available in the United States
- No effective vaccines or treatments exist
- There are at least two strains of the virus circulating and it continues to mutate
- There is conflicting evidence regarding immunity from past exposures
- The disease continues to stress our hospital systems, healthcare workers, and is resulting in reduced health care for other diseases
Emerging Medical Issues Regarding COVID-19
- There is an expanding range of symptoms associated with COVID-19 attacking distinct body systems. This is uncharacteristic of coronaviruses: several are potentially fatal and the long-term effects of non-fatal exposures are unknown. These symptoms include:
- Respiratory inflammation and pulmonary embolisms
- Unexpected blood clotting
- Strokes
- Weakened heart muscles and arrythmias
- Kidney damage
- Immune system impacts
- A multi-system inflammatory syndrome threatening young people
Pressures to Reopen America
- Between twenty and thirty million Americans are now unemployed
- There are adverse health effects associated with unemployment
- The Congress has invested more than $2 trillion in emergency funds without clear effect
- Many businesses forced to close will not be able to reopen
- The longer the economy is shut down the harder it will be to reopen
+ + +
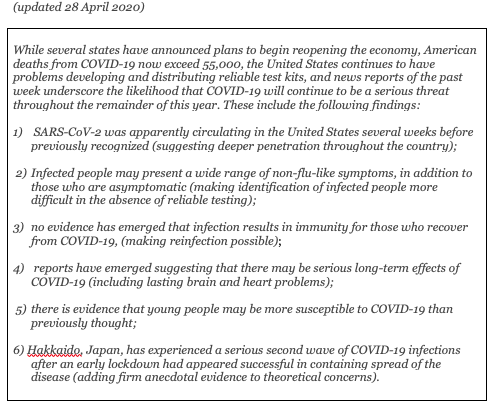
[update: May 4, 2020] As states begin relaxing COVID-19 restrictions rowing teams and clubs consider appropriate safety precautions, it is important to recognize that much of our knowledge of the disease remains tentative: our understanding of infection rates, transmission vectors, death rates, symptoms, lasting effects, comorbidity factors, immunity, are all under continuing review and subject to continuing revisions.
+ + +
SARS-CoV-2 — the virus causing the disease — is clearly an infectious and potentially lethal virus. It appears clear that it can be transmitted through from person to person through the aerosols of normal respiration (coughing, sneezing, normal breathing), and through contact with common surfaces (door handles, oar handles, cells phones, boats, etc.) And it is clear that no reliable tests, treatments or vaccines are available yet to control the disease and prevent its transmission.
The virus is also a moving target: it can change as quickly as our scientific advances or social habits. There appear to be two variants of the virus currently circulating, there is a widespread consensus among epidemiologists that a “second-wave” of infections is likely to occur later this year, and there is no way of predicting whether or not this will coincide with an aggressive influenza season.
These are cautionary notes. The number of confirmed cases in the US is now over one million and medical experts continue to warn that the threats of infection, serious disease, and death still remain. As we resume rowing, we should keep these facts in mind.
*
Social distancing is only a mechanism for flattening the curve of infection in a population. It provides only limited protection to individuals in a group.
*
An Overview
The COVID-19 pandemic* poses a unique threat to all of us. The most important issues of rowing safety at the moment involve life and death questions of virology and epidemiology for which no one knows the answers. The science is preliminary and fast-moving; the anecdotal information alternately frightening, hopeful, conflicting, and uncertain. The political and institutional responses have been dramatic and affected all aspects of the American economy and social life.
In the six-week period between March 1st, when the first COVID-19 death in the United States was confirmed, and April 15th, more than a half million Americans were infected and more than 26,000 Americans died from the disease. Nothing has killed more Americans more quickly since the Battle of Gettysburg in 1863.
At this time there continues to be a shortage of tests kits in the United States, there is no effective treatment and no vaccine, and it is expected that a second wave of infections is likely to occur in the fall. Symptoms can vary widely, infected people may be asymptomatic, and the disease is highly infectious: it can be transmitted by surface contact or the aerosols of normal coughing, sneezing, and breathing. Prematurely resuming normal social activities will be risky.
The United States is now the epicenter for the worldwide pandemic, having lagged behind other nations both in developing and accessing test kits and in effective political actions. Everyone’s lives have been disrupted by this disease. The COVID-19 pandemic poses a dilemma shared by all Americans: when can we resume normal activities?
For many rowers the question is When Can We Row Again?
There is no clear answer. The 2020 Olympics have been postponed until 2021; FISA/World Rowing has cancelled all events through the end of the year; USRowing’s youth events have also been cancelled. Most states have imposed limitations on social activities and sports events to limit spread of the disease. As these restrictions ease, individuals and clubs must make their own decisions about rowing before the virus is under control. There is a growing consensus among epidemiologists about what should be done to before resuming normal activities, but it is at odds with conflicting political interests.
More information is available on RowSafeUSA.Org and will continue to be updated.
Ten Facts You Should Know Before Resuming Rowing
1. COVID-19 is a new disease. Human beings have no immunity for this disease. There are no effective treatments, no vaccines, and the United States continues to lag in the development and distribution of test kits necessary to contain the disease.
2. COVID-19 is highly contagious. The disease can be spread through direct contact between human beings or surface contact with contaminated objects. The primary vector, however, is through the aerosols dispersed in normal breathing, coughing, and sneezing, which may be spread up to twenty feet or more and remain airborne for hours. Most face masks do not prevent the virus from entering your nose and mouth but can reduce the risk. For this reason it is essential to wash frequently with soap and water.
3. COVID-19 symptoms vary widely and carriers may be asymptomatic. The most common symptoms resemble common diseases: fever: fatigue, cough, aches and pains, runny nose, sore throat, and shortness of breath. As many as half of all infected people may show no symptoms but still transmit the disease.
4. COVID-19 is deadly. Between March 1st and April 20th more than 40,000 Americans died from the disease. That is greater than the number of American combat soldiers who died in Vietnam from 1965 through 1968 (36,340) and the number who died on D-Day in World War II (6,603). More Americans are now dying daily from COVID-19 than died on 9/11.
5. The United States is now the epicenter of this global pandemic. It has had more cases of COVID-19 (>750,000) and more deaths (>40,000) than any other county and these numbers are continuing to rise. There is no indication it is subsiding or under control.
6. All COVID-19 data is preliminary and may underestimate the actual numbers. Because the disease is so new, all numbers regarding infections and deaths are subject to revision. Because so many people appear to be asymptomatic, or have mild symptoms, there are likely to be many more carriers of the disease than the confirmed number of cases indicate. Similarly, deaths from pneumonia and other respiratory diseases may conceal more deaths linked to COVID-19.
7. Social Distancing doesn’t prevent COVID-19 transmission. It reduces the risk. Models of aerosol dispersion for runners, cyclists, and from coughing and sneezing indicate viral droplets may extend twenty to twenty-five feet from their source.
8. Exercise strengthens immunity. Because the white blood cells and proteins used to rebuild muscles after strenuous workouts are also used to fight diseases, exercise is generally healthy and bolsters immunity. Overexertion, however, without allowing recovery time, may weaken immunity.
9. There is likely to be a second wave of infections. Viruses persist and mutate. In the absence of an effective vaccine epidemiologists expect there is likely to be a second wave of infections (and deaths) in the fall. It is possible, as was the case with the flu epidemic of 1918-19, that the virus may become more lethal as a result of mutations.
10. All COVID-19 numbers are estimates and we have no facts about the future. All numbers of reported cases and deaths are estimates drawn from varying sources and tend to underestimate the actual numbers. No one can predict the future of this disease but there seems to be a growing consensus among epidemiologists of four steps necessary to control it:
1) we must test widely for COVID-19;
2) everyone who tests positive or shows symptoms must be isolated;
3) everyone who has been in contact with infected people must be located; and
4) infected people and everyone who has been in contact with them must be quarantined for 14 days.
The Emergence of COVID-19 in China
COVID-19 emerged in a remote part of China in late 2019 and began to spread through the population for several weeks before its first detection and recognition as a new viral disease. On December 31st the government of China reported a cluster of forty-one patients exhibiting the apparently new viral disease. On January 11th China reported its first death from the disease. On January 13th the first case was reported outside of China. On January 20th the first case reported in the United States was a 35-year old man in Snohomish County, Washington.
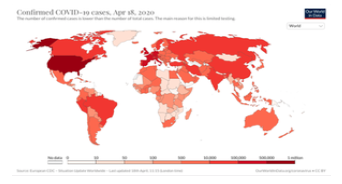
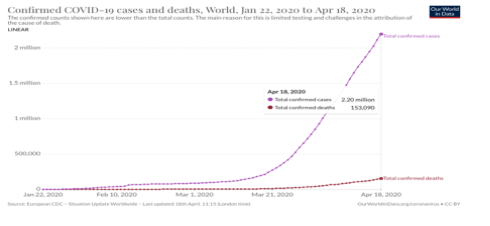
By mid-April there have been more than two million confirmed cases of the disease throughout the world. The greatest number of these cases are now in the United States.
Globally, more than 150,000 people have died and the end is not yet in sight. In the United States more than 40,000 have died.
Confirmed Infections and Deaths in the United States
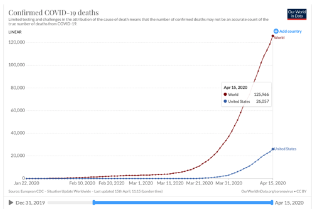
By mid-April the United States was reporting more deaths from COVID-19 than any other country, as shown here in comparison with Italy, Spain, the UK, Germany, China and South Korea. Particularly noteworthy is a comparison of the slopes between the United States, Europe, South Korea, and China.
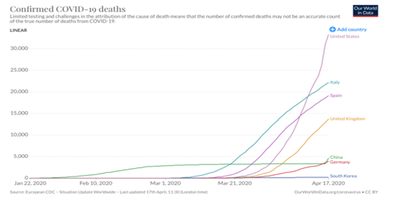
While the number of confirmed deaths in China grew gradually in February it had leveled off by March. In South Korea the slope has remained low and flat. In contrast the increased number of deaths in the United States, UK, Italy, Spain, and Germany all began approximately two or three weeks after China had brought its death rate under control, and all have risen sharply without yet leveling.
A simplified comparison between the United States (and Europe) and China (and South Korea) looks like this.
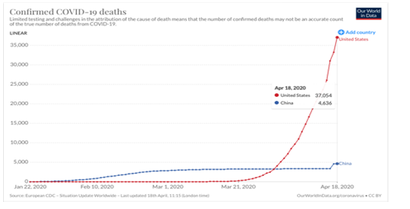
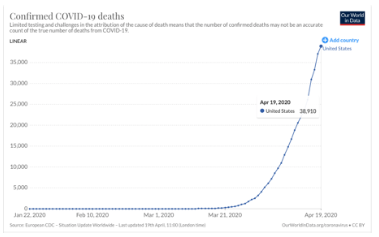
Between Easter Sunday and the following Sunday, April 19th, the death toll in the United States rose from slightly more than 20,000 to more than 38,000.
The sharp growth in US COVID-19 deaths reflects a comparable growth in the number of confirmed infections, which is approaching 750,000.
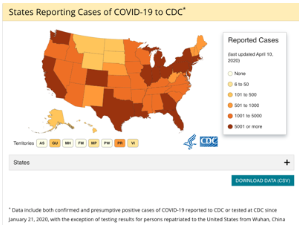
A distribution map of the United States indicates that the disease has already spread to all fifty states,
and several analyses indicate that areas currently with low infection (and mortality) rates may be at high risk in the coming months.
As of April 20th, the United States remains the epicenter of the world pandemic while all three of these trends continue. As the number of infections continue to spread further into rural areas of the United States, the number of infections and the number of deaths continue to rise.
The Science
Science provides no clear or simple answers regarding the future course of this pandemic. Viruses are among the oldest living things on earth, although they don’t conform to conventional definitions of life. They are parasitic bits of genetic material encapsulated in protein coats, without cellular structure or the normal attributes of life forms. Yet there appear to be millions of types of viruses in virtually all of the world’s ecosystems and scientists have categorized approximately 5,000 distinct “species”, of which the coronavirus is one.
The question is inherently complex. Science is a process in which knowledge emerges only through trial and error; through the accumulation of data, the development of hypotheses, and the constant re-evaluation of both. New evidence, much like old assumptions, often prove to be misleading. And in the case of viral epidemics such as this, the enemy – in this case the SARS-CO-2 virus – is a moving target. In fact, as of this writing, it already exists in two identified variations, one of which is thought to be more lethal and the other, perhaps, more threatening.**
Those with compromised immunity and existing respiratory or heart conditions appear to be at greatest risk, and men appear to be at great risk than women. Those over the age of sixty have been most vulnerable and those under the age of thirty least likely to die, but people of all ages have died.
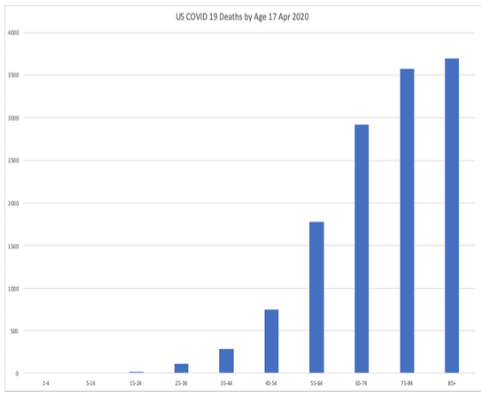
Reportedly healthy individuals under the age of thirty have succumbed quickly to the disease.
Combatting the pandemic involves several distinct branches of science. Most prominent in the public discourse so far has been epidemiology, or the study of disease emergence, transmission, and control in populations. With COVID-19 the epidemiology began with the observation of a novel flu-like virus emerging in Wuhan, China, in the late fall of 2019. Assuming the virus emerged as a human disease after adapting from some other animal (suspected to have been bats sold in China’s live meat markets), presumably it would have been transmitted among humans before it could have been identified as a newly emerging disease. In part for this reason, as Chinese doctors began identifying and treating the disease, it would already have been spreading, while its potential lethality would have been debated.
The Politics
The recent decisions of elected officials to effectively shut down normal social operations, closing schools, curtailing business operations, and restricting social gatherings, are unprecedented in American peacetime. With few exceptions they have probably been both legal and constitutional.
Political decisions are necessarily guided by a wide range of considerations. These extend beyond science and medicine – both of which include uncertainties about the current disease and projections of its course — and they reflect on the nature of risk management. Political decisions affecting the economy and people’s livelihoods must be based on imperfect and conflicting information.
Once the first reports of the emerging disease began to reach government health officials, decisions were made to assess the nature of the disease itself, available diagnostic tools, potential therapeutic tools, and appropriate political actions. As documents become available the various ways in which these decisions have affected the course of the disease in the United States are becoming more apparent. While information was becoming available and being assessed by government decision-makers, the disease continued to spread. In retrospect it is becoming increasingly clear that early signs of the disease’s severity were under-estimated and both important decisions and actions were delayed.
The following timeline provides a framework for analyzing the nature of information and risk mitigation in the course of the COVID-19 pandemic to date.
COVID-19 Timeline
This timeline is based on timelines prepared by the New York Times and Washington Post and supplemented with more recent news reports cited in the endnotes. WH refers to statements issued by the White House; CDC to the Center for Disease Control and Prevention; NIAID to the National Institute of Allergy and Infectious Diseases; WHO to the World Health Organization.
20 Apr CDC reports 39,084 deaths in US; 756,625 confirmed cases in US.
19 Apr US Death Toll 38,910. Confirmed cases 735,086
12 Apr Easter Sunday, President Trump’s initial target date for re-opening American economy: US Death toll 20,600.
07 Apr US death toll exceeds 10,500
31 Mar US Death toll from COVID-19 surpasses death toll of 9/11
30 Mar VA, MD, & DC issued orders requiring residents to stay at home.
29 Mar President Trump extends national shutdown through April 30th acknowledging US death toll could surpass 100,000.
28 Mar CDC urged residents of NY, NJ, and CT to refrain from non-essential travel
27 Mar President Trump signs $2.2 trillion stimulus package into law.
26 Mar The US officially became the country hardest hit by COVID-19, with more than 80,000 confirmed cases and more than 1,000 related deaths.
24 Mar President Trump announces “I’d love to have the country opened up and just raring to go by Easter.” Tokyo Olympics postponed.
17 Mar President Trump: “I felt it was a pandemic long before it was called a pandemic.” [US deaths total 108]
16 Mar President Trump recommends gathering of less than 10 people.
15 Mar CDC recommends gatherings of no more than 50 people.
15 Mar President Trump: “This is a very contagious virus. It’s incredible. But it’s something we have tremendous control over.” [US deaths total 63]
13 Mar President Trump declares a national emergency.
10 Mar President Trump: “We’re prepared, and we’re doing a great job with it. And it will go away. Just stay calm. It will go away.”
06 Mar Epidemiologists warn WH epidemic could resemble 1918 Influenza infecting more than 80% of Americans with more than 2 million deaths. [US death total: 11]
04 Mar President Trump: “Some people will have this at a very light level… There are many people like that.” [US deaths total 28]
03 Mar Ninth US death occurs; CDC lifts restrictions on COVID-19 testing. [US death total: 9]
29 Feb WH warns against travel to certain countries. First death is reported in the United States.
28 Feb President Trump: “It’s going to disappear. One day, it’s like a miracle, it will disappear.” First US death reported.
24 Feb WH requests $1.25 billion for Covid-19
24 Feb President Trump: “The Coronavirus is very much under control in the USA… Stock Market starting to look very good to me!”
10 Feb President Trump predicts “Looks like by April… it miraculously goes away.”
07 Feb Dr. Li Wen Liang dies of Covid-19 after having tried to raise early alarms and being reprimanded by Chinese government.
02 Feb First confirmed death outside China.
31 Jan US restricts travel from China.
30 Jan WHO declares global health emergency.
29 Jan WH advisor Peter Navarro warns COVID-19 threatened millions of Americans and could cost trillions of dollars.
22 Jan President Trump assures nation “We have it totally under control… It’s going to be just fine.”
21 Jan First confirmed case in U.S.
11 Jan First confirmed death in China.
07 Jan The coronavirus disease (COVID-2019) was identified as the causative virus*** by Chinese authorities on 7 January (2020).
Dec, 2019 On 31 December 2019, WHO was informed of a cluster of cases of pneumonia of unknown cause detected in Wuhan City, Hubei Province of China.
2019 US President Donald Trump eliminated a key American public health position in Beijing that was intended to help detect disease outbreaks in China.
2018 President Trump disbands National Security Council pandemic response team (the Global Health Security and Biodefense Unit).
Jan, 2017 National Security Council briefs WH on “Early Response to High-Consequence Emerging Infectious Disease Threats.”
Jan, 2017 Dr. Anthony Fauci warned on 19 January, 2017, in a speech titled “Pandemic Preparedness in the Next Administration that an infectious epidemic was likely to occur and listed necessary measures to prepare for such an epidemic.
Jan, 2017 Several days before taking office, Donald Trump’s staff was briefed by outgoing administration officials about preparedness for a possible influenza pandemic.
Jan, 2017 The Pentagon prepared a draft plan for “Pandemic Influenza and Infectious Disease Response,” specifically noting “The most likely and significant threat is a novel respiratory disease, particularly a novel influenza disease,” specifically identifying the potential shortages of respiratory masks, ventilators and hospital beds.
* COVID-19 is the official terminology of the World Heal Organization referring to the viral disease that was identified in late 2019. It is an acronym for COrona VIrus Disease-2019. The virus that causes the disease is referred to as SARS-COV-2, An acronym for Severe Acute Respiratory Syndrome – COronaVirus -2.
** Because viruses are parasitic and cannot exist without hosts, a virus which is so lethal that it kills it host before it can move to another is less likely to survive. A virus which may be debilitating to its host, and lethal to only a limited percentage of its hosts, is more likely to be transmitted from one host to another and spread more widely. There is some evidence the COVID-19 virus currently exists in both forms.
***See footnote * above regarding terminology
© 2020 RowSafeUSA.Org
