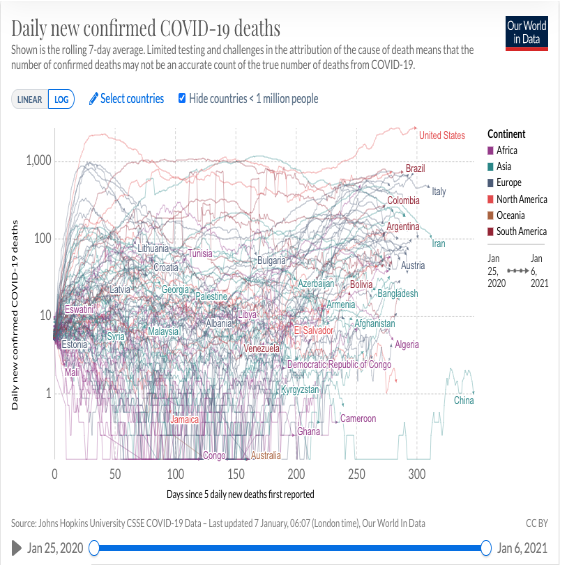
“The United States and many parts of the world have now lost control of the Covid-19 pandemic owing to the respiratory spread of SARS-CoV-2 and to inconsistent adherence to effective public health measures, including wearing masks and maintaining social distancing. Persons infected with SARS-CoV-2 are frequently asymptomatic, yet they have high respiratory viral loads, and they are major purveyors of viral spread. These factors have led to the current explosion of Covid-19 hospitalizations and deaths, with Covid-19 now a major cause of death in the United States. Our only hope is safe and effective vaccines that can be widely deployed to provide herd immunity that can control viral spread.” [Haynes, Barton F., “A new Vaccine to Battle Covid 19,” New England Journal of Medicine, 4 February 2021, https://www.nejm.org/doi/full/10.1056/NEJMe2035557?query=TOC ]
——-
COVID-19 remains the foremost rowing safety concern as we head into the new year. In addition to the record-breaking numbers of infections and deaths in the United States and their impacts on emergency medical services, concerns continue to grow regarding the new variants that are emerging. This past week Britain imposed its most stringent lockdown since last March due to concerns about the highly contagious new variant (with twenty mutations) circulating in England and already detected in United States.
3,964 new COVID-19 deaths were reported in the US on Wednesday, January 6th, along with 255,000 new cases.
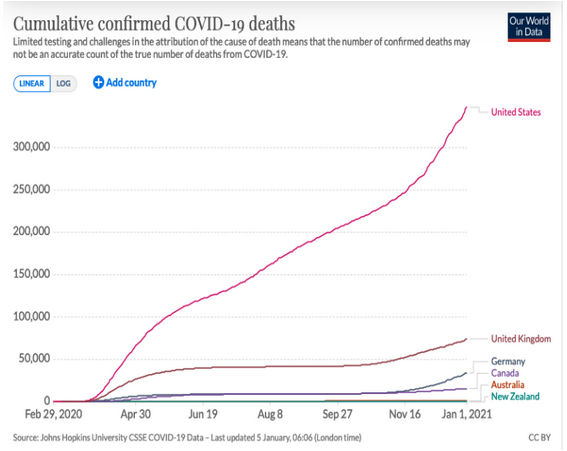
COVID-19 remains a serious safety risk for rowers as the United States continues to have one of the highest numbers of confirmed deaths, the highest number of confirmed cases, and the highest numbers of cases and deaths per capita, among the countries of the world.
At the same time the COVID-19 virus continues to mutate; it has become apparent that it can infect people of all ages, including healthy young adults; and there may be long-term cognitive effects from even mild infections.
It is not clear what this means for rowing competitions in the coming year.
[Editor’s note: In late July the New York Times reported that one-third of the US women’s national team had contracted the COVID-19 virus at its New Jersey training camp in March. Beyond this update, however, we have left the page unchanged since it was posted in April to illustrate how much basic information was available early in the pandemic’s emergence. The numbers continue to change, but the basic facts haven’t. Additional COVID-19 information is available here on other pages.]
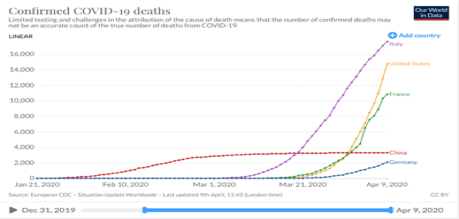
The COVID-19[i] pandemic poses a unique threat to all of us. The most important issues of rowing safety at the moment involve life and death questions of virology and epidemiology for which no one knows the answers. The science is preliminary and fast-moving; the anecdotal information alternately frightening, hopeful, conflicting, and uncertain. Following are key points to keep in mind, plus links to CDC, WHO, FISA, and USRowing.
1. COVID-19 is a novel coronavirus: The fact that this is novel is important. Viruses are microscopic parasites[ii] that change continuously,[iii] may move from one species (e.g., bats or monkeys) to another species (i.e. humans).[iv] In rare instances they can and do cause disease when they jump from one species to another.[v] That is what has happened with the emergence of COVID-19. Although it is part of a large family of coronaviruses that are familiar to humans, and for which we have developed immunities, humans have no immunity to this newly emerged virus.
2. Contagion and Infection: All viruses require two things: hosts (in which they replicate) and vectors (to move from one host to another). They cannot survive without both. In order to survive and cause disease viruses must move from one host to another (contagion) and disrupt the host’s normal functioning (infection). In humans (and birds) coronaviruses generally cause respiratory infections and are transmitted in droplets from coughing and sneezing.[vi]They can survive for hours or days (or longer?) outside of hosts and they can be transmitted through physical contacts. These characteristics vary with each strain of virus and are not completely understood yet for COVID-19.
3. Exercise & Immunity: Among the many ways in which exercise is healthy is the fact that it can bolster the immune system. Or it can weaken it, depending in large part on the patterns of stress and recovery in your workouts.[vii]Because the white blood cells and proteins used to rebuild muscles after strenuous workouts are used to fight diseases, proper exercise helps build health immune systems. “However,” Dr. Gabe Mirkin reports, “several recent studies show that if you don’t follow your hard workouts with easy ones, you may suppress your immune system (and) increase risk for developing infections such as colds…”[viii] Naturally, you should not exercise if you feel sick.[ix]
4. Social Distancing: The Center for Disease Control and Prevention (CDC) has recommended maintaining distances of at least six feet between individuals – including those who show no symptoms of disease – to control the spread of COVID-19.[x] This is based largely on the theory that virus containing particles from normal breathing are unlikely to travel that distance[xi] and advice from the World Health Organization (WHO) based on evidence from China.[xii]
5. Social Isolation: In contrast to social distancing, recent reports from China[xiii] and a more recent report from a town in Italy,[xiv] have suggested that severe social lockdowns – restricting all non-essential human contacts – combined with comprehensive testing, can effectively control spread of the virus.
6. Aerosol Infection: On March 30th the LA Times reported that 45 out of 60 people attending a choir practice in Mount Vernon, Washington, on March 6th had contracted COVID-19 and two had died – despite the fact that no one in attendance had appeared symptomatic and recommended safety precautions in effect had been strictly observed.[xv] This is contrary to WHO’s reading of the evidence from China.[xvi]
7. Who is at risk? Everyone. Almost half of the COVID-19 hospitalizations in the United States have been for people below the age of 40,[xvii] including fatalities below the age of 20.[xviii]
Percentage Fatalities by Age (CDC based on Chinese Data)[xix]
Due to the preliminary nature of the available data there doesn’t yet seem to be a consensus about the fatality rate associated with COVID-19;[xx] however, there does appears to be a consensus that it is both significantly more contagious than the seasonal flu and has a higher fatality rate. In the United States the CDC estimates approximately 60,000 deaths annually from influenza[xxi],with annual numbers ranging from 12,000 to 79,000 deaths.[xxii] The CDC has advised that people over the age of 65 and those with serious underlying health issues are at greatest risk from COVID-19.[xxiii] As more data accumulates in the United States, however, there have been reports of people without other serious medical risks of all ages having died from COVID-19.[xxiv]
8. There is no vaccine and no effective treatment for COVID-19 at this time. On March 30 the Federal Drug Administration (FDA) took the unusual step of authorizing the use of an unproven drug for treatment of the disease.[xxv]
9. The difference between COVID-19 and the flu: Hugh Montgomery, Professor of Intensive Care at University College London, offers a very clear explanation of the why COVID-19 is so dangerous.[xxvi]
10. Further Reading: There are many books on infectious diseases, among which Plagues and People, by William H. McNeill, (Penguin Random House, 1977, remains a foundational book on the subject. It is dense reading. More current and probably more accessible to most readers, including myself, is The Great Influenza, by John M. Barry, (Viking, 2004).
For more information:
National Center for Disease Control (CDC)
https://www.cdc.gov/coronavirus/2019-ncov/index.html
World Health Organization (WHO) https://www.who.int/emergencies/diseases/novel-coronavirus-2019
FISA (Federation Internationale des Societes d’Aviron)
http://www.worldrowing.com/news/update-the-coronavirus-covid
USRowing
https://usrowing.org/sports/2020/3/4/usrowing-coronavirus-information-and-updates.aspx
[i] COVID-19 is sometimes referred to as SARS-CoV-2; COVID-19 referring specifically to the disease associated with the corona virus that emerged in 2019.
[ii] https://www.livescience.com/53272-what-is-a-virus.html
[iii] https://www.ncbi.nlm.nih.gov/books/NBK8439/
[iv] https://en.wikipedia.org/wiki/Cross-species_transmission
[v] https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html
[vi] https://en.wikipedia.org/wiki/Coronavirus
[vii] https://www.drmirkin.com/fitness/how-exercise-affects-your-immunity.html
[viii] ibid
[ix] https://webmail.earthlink.net/wam/msg.jsp?msgid=43678&folder=INBOX&isSeen=false&x=1162367384
[x] https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html
[xi] https://www.nejm.org/doi/full/10.1056/NEJMc2004973?query=RP
[xii] https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
[xiii] citation needed
[xiv] “Frequently Asked Questions About Estimated Flu Burden,” CDC, https://www.cdc.gov/flu/about/burden/faq.htm#deaths
[xv] Coronavirus Disease 2019 (COVID-19): People who are at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fspecific-groups%2Fhigh-risk-complications.html
[xvi] citation needed
[xvii] Pam Belluck, “Young Adults Make Up Big Portion of Coronovirus Hospitalizations in U.S.,” New York Times, 18 March 2020. https://www.nytimes.com/2020/03/18/health/coronavirus-young-people.html?action=click&module=RelatedLinks&pgtype=Article
[xviii] Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19),” CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
[xix] “Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19),” CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
[xx] Dimple, Rajgor, D., et al. “The many estimates of the COVID-19 case fatality rate,” The Lancet, 27 March, 2020. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30244-9/fulltext
[xxi] citation needed
[xxii] “Frequently Asked Questions About Estimated Flu Burden,” CDC, https://www.cdc.gov/flu/about/burden/faq.htm#deaths
[xxiii] Coronavirus Disease 2019 (COVID-19): People who are at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fspecific-groups%2Fhigh-risk-complications.html
[xxiv] citation needed
[xxv] Christopher Rowland, “FDA authorizes widespread use of unproven drugs to treat coronavirus, saying possible benefit outweighs risk,” Washington Post, 30 March 2020. https://www.washingtonpost.com/business/2020/03/30/coronavirus-drugs-hydroxychloroquin-chloroquine/.
[xxvi] https://www.youtube.com/watch?v=Sg7RnPPKN48
